Cardiovascular Disease Risk Calculator
Cardiovascular Disease Risk Calculator
Instructions
This calculator should be used for primary prevention patients (those without ASCVD) only.
How to use the calculator:
- Enter the information to all of the fields.
- Click Calc button to get the result.
- If all of the fields have not been filled, or the values outside the ranges, the calculator will not run; and instead, errors will be prompted. Please correct the errors and try again.
- The Calculator is valid only for age of 40 to 79 years old, total cholesterol of 130 to 320 mg/dL, HDL cholesterol of 20 to 100 mg/dL, and systolic blood pressure of 90 to 200 mmHg.
- Click Reset button will clear all of the entries. It is a good practice to press Reset button before entering the information.
- If you want to copy the information to your note, click the Copy button, which will copy the information to the clipboard. Then, in your note, press Ctrl+V , which will pastes the copied information to your note.
This calculator is based on ASCVD Pooled Cohort Risk Equations (Goff 2013) as of the following:
- Terms = (C_Age * ln(Age)) + (C_Sq_Age * sq(ln(Age))) + (C_Total_Chol * ln(Total_cholesterol)) + (C_Age_Total_Chol * ln(Age) * ln(Total_cholesterol)) + (C_HDL_Chol * ln(HDL_cholesterol)) + (C_Age_HDL_Chol * ln(Age) * ln(HDL_cholesterol)) + (On hypertension medication * C_On hypertension medications * ln(Systolic blood pressure)) + (On hypertension medication * C_Age_On hypertension medications * ln(Age) * ln(Systolic blood pressure)) + (not On hypertension medication * C_Off_Hypertension_Meds * ln(Systolic blood pressure)) + (not On hypertension medication * C_Age_Off_Hypertension_Meds * ln(Age) * ln(Systolic blood pressure)) + (C_Smoking * Smoking) + (C_Age_Smoking * ln(Age) * Smoking) + (C_Diabetes * Diabetes)
- 10-year risk = 100 * (1 - S10e(Terms-Mean_Terms))
- Calculation details and variables
- For Black or African American female patients CAge = 17.114; CSqAge = 0; CTotalChol = 0.94; CAgeTotalChol = 0; CHDLChol = -18.92; CAgeHDLChol = 4.475; COnHypertensionMeds = 29.291; CAgeOnHypertensionMeds = -6.432; COffHypertensionMeds = 27.82; CAgeOffHypertensionMeds = -6.087; CSmoking = 0.691; CAgeSmoking = 0; CDiabetes = 0.874; S10 = 0.9533; MeanTerms = 86.61.
- For White or other race female patients CAge = -29.799; CSqAge = 4.884; CTotalChol = 13.54; CAgeTotalChol = -3.114; CHDLChol = -13.578; CAgeHDLChol = 3.149; COnHypertensionMeds = 2.019; CAgeOnHypertensionMeds = 0; COffHypertensionMeds = 1.957; CAgeOffHypertensionMeds = 0; CSmoking = 7.574; CAgeSmoking = -1.665; CDiabetes = 0.661; S10 = 0.9665; MeanTerms = -29.18.
- For Black or African American male patients CAge = 2.469; CSqAge = 0; CTotalChol = 0.302; CAgeTotalChol = 0; CHDLChol = -0.307; CAgeHDLChol = 0; COnHypertensionMeds = 1.916; CAgeOnHypertensionMeds = 0; COffHypertensionMeds = 1.809; CAgeOffHypertensionMeds = 0; CSmoking = 0.549; CAgeSmoking = 0; CDiabetes = 0.645; S10 = 0.8954; MeanTerms = 19.54.
- For White or other race male patients CAge = 12.344; CSqAge = 0; CTotalChol = 11.853; CAgeTotalChol = -2.664; CHDLChol = -7.99; CAgeHDLChol = 1.769; COnHypertensionMeds = 1.797; CAgeOnHypertensionMeds = 0; COffHypertensionMeds = 1.764; CAgeOffHypertensionMeds = 0; CSmoking = 7.837; CAgeSmoking = -1.795; CDiabetes = 0.658; S10 = 0.9144; MeanTerms = 61.18.
This calculator helps predict the 10-year risk of the following hard ASCVD events:
- First occurrence of nonfatal myocardial infarction
- CHD death
- Fatal or nonfatal stroke
This calculator may overestimate risk and a discussion with the patient needs to ensue if there are any questions.
Risk estimates were developed from cohorts primarily comprising White and African American subjects. Risk may be underestimated in Native Americans, Asian Americans of South Asian ancestry, and Puerto Ricans. Risk may be overestimated in Asian Americans of East Asian ancestry and some Mexican Americans.
Advice
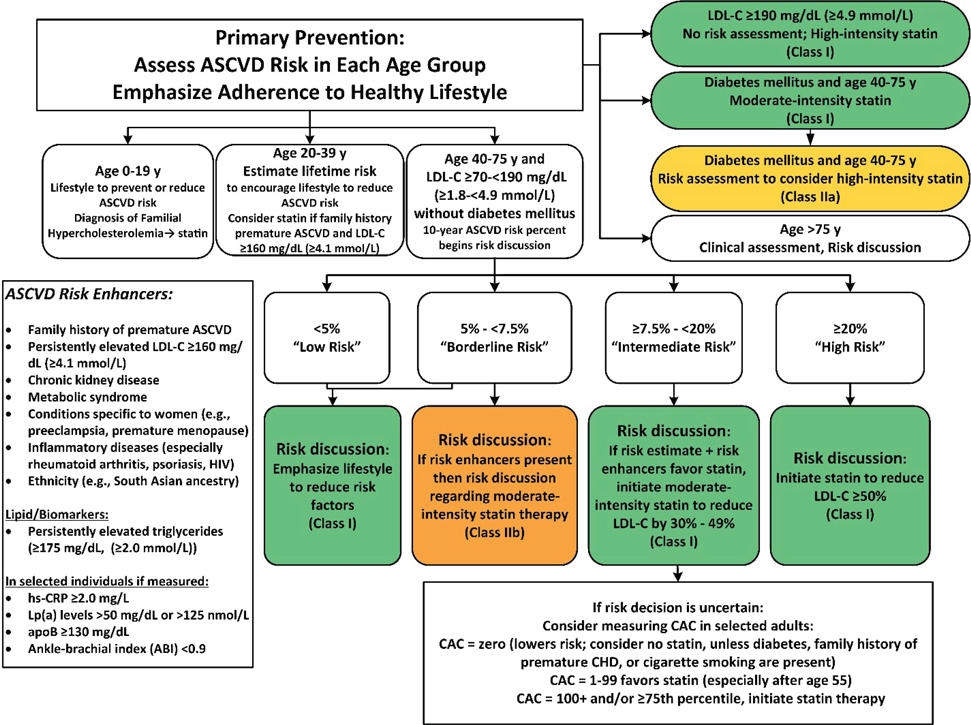
When Considering Starting Statins
Always engage in a clinician-patient discussion of the potential for ASCVD risk reduction, adverse effects, drug-drug interactions, and patient preferences. Consider:
- Potential for ASCVD risk-reduction benefits.
- Potential for adverse effects and drug-drug interactions.
- Heart-healthy lifestyle.
- Management of other risk factors.
- Patient preferences.
Statin therapy is not routinely recommended for individuals with New York Heart Association class II to IV heart failure or who are receiving maintenance hemodialysis.
When Considering or Using High-Intensity Statins
The guidelines recommend the treating clinician consider:
- Multiple or serious comorbidities, such as impaired renal or hepatic function.
- A history of previous statin intolerance or muscle disorders.
- Unexplained elevated levels of alanine transaminase greater than three times the upper limit of normal.
- Patient characteristics or concomitant use of medications that affect statin metabolism.
- Age older than 75 years.
When Considering Other Groups for Aggressive Cholesterol-Lowering Medications Besides Those in the Risk Calculator
The guidelines recommend the treating clinician consider patients with:
- A primary LDL-C level of 160 mg per dL (4.14 mmol per L) or greater, or other evidence of genetic hyperlipidemias.
- Family history of premature ASCVD before 55 years of age in a first-degree male relative or before 65 years of age in a first-degree female relative.
- High-sensitivity C-reactive protein level of 2 mg per L (19.05 nmol per L) or greater.
- Coronary artery calcium score of 300 Agatston units or greater, or being in the 75th percentile or greater for age, sex, and ethnicity.
- Ankle-brachial index (ABI) less than 0.9.
- Elevated lifetime risk of ASCVD.
When Monitoring Statin Effects and Side Effects
- Assess adherence, response to therapy, and adverse effects within 4 to 12 weeks following statin initiation or change in therapy.
- Measure fasting lipid levels.
- Do not routinely monitor alanine transaminase or creatine kinase levels unless symptomatic.
- Screen and treat type 2 diabetes according to current practice guidelines; heart-healthy lifestyle habits should be encouraged to prevent progression to diabetes.
Action
Use for Guiding Statin Use (Arnett 2019)
| Risk Score | Severity | Risk Discussion |
|---|---|---|
| <5% | Low Risk | Emphasize lifestyle to reduce risk factors |
| 5-<7.5% | Borderline Risk | If risk enhancers present, then risk discussion regarding moderate-intensity statin therapy |
| ≥7.5-<20% | Intermediate Risk | If risk estimate + risk enhancers favor statin, initiate moderate-intensity statin to reduce LDL-C by 30 to 49% If risk decision is uncertain, Consider measuring Coronary Artery Calcium (CAC) in selected adults: CAC = zoro (lowers risk; consider no statin, unless diabetes, family history of premature CHD, or cigarette smoking are present); CAC = 1-99 favors statin (especially after age 55); CAC = 100+ and/or ≥75th percentile, initiate statin therapy. |
| ≥20% | High Risk | Initiate statin to reduce LDL-C ≥50% |
ASCVD Risk Enhancers:
- Family history of premature ASCVD
- Persistently elevated LDL-C ≥160 mg/dL
- Chronic kidney disease
- Metabolic syndrome
- Conditions specific to women (eg, preeclampsia, premature menopause)
- Infammatory disease (especially rheumatoid arthritis, psoriasis, HIV)
- Ethnicity (eg, South Asian ancestry)
Lipid/Biomarkers:
- Persistently elevated triglycerides (≥175 mg/dL)
In selected individuals if measured:
- hs-CRP (≥2.0 mg/L)
- Lp(a) level (≥50 mg/dL)
- apoB (≥130 mg/dL)
- Ankle-brachial index (ABI) <0.9
Use for Guiding Blood Pressure Control (Whelton 2018)
| Risk Score | Target Blood Pressure | Comment |
|---|---|---|
| <10% | 140/90 mmHg | Use of blood pressure-lowering medication is recommended for primary prevention of CVD in adults with no history of CVD and with an estimated 10-year ASCVD risk <10% and blood pressure ≥140/90 mmHg. |
| ≥10% | 130/80 mmHg | Use of blood pressure-lowering medications is recommended for primary prevention in adults with an estimated 10-year ASCVD risk of ≥10% and blood pressure ≥130/80 mmHg. |
Statin Therapy
| Intensity | LDL Lowering | Medication (mg/day) |
|---|---|---|
| High | ≥50% | Atorvastatin 40–80; Rosuvastatin 20-40 |
| Moderate | 30% to <50% | Atorvastatin 10-20; Rosuvastatin 5-10; Simvastatin 20–40; Pravastatin 40-80; Lovastatin 40; Fluvastatin 80 (IR BID dosing); Pitavastatin 2–4 |
| Low | <30% | Simvastatin 10; Pravastatin 10–20; Lovastatin 20; Fluvastatin 20–40; Pitavastatin 1 |
Reference
Goff DC Jr, Lloyd-Jones DM, Bennett G, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2014 Jun 24;129(25 Suppl 2):S74-5]. Circulation. 2014;129(25 Suppl 2):S49-S73. doi:10.1161/01.cir.0000437741.48606.98Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines [published correction appears in Circulation. 2014 Jun 24;129(25 Suppl 2):S46-8] [published correction appears in Circulation. 2015 Dec 22;132(25):e396]. Circulation. 2014;129(25 Suppl 2):S1-S45. doi:10.1161/01.cir.0000437738.63853.7a
Ridker PM, Cook NR. Statins: new American guidelines for prevention of cardiovascular disease. Lancet. 2013;382(9907):1762-1765. doi:10.1016/S0140-6736(13)62388-0
Chia YC, Lim HM, Ching SM. Validation of the pooled cohort risk score in an Asian population - a retrospective cohort study. BMC Cardiovasc Disord. 2014;14:163. Published 2014 Nov 20. doi:10.1186/1471-2261-14-163
Rana JS, Tabada GH, Solomon MD, et al. Accuracy of the Atherosclerotic Cardiovascular Risk Equation in a Large Contemporary, Multiethnic Population. J Am Coll Cardiol. 2016;67(18):2118-2130. doi:10.1016/j.jacc.2016.02.055
Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Circulation. 2019 Sep 10;140(11):e647-e648] [published correction appears in Circulation. 2020 Jan 28;141(4):e59] [published correction appears in Circulation. 2020 Apr 21;141(16):e773]. Circulation. 2019;140(11):e563-e595. doi:10.1161/CIR.0000000000000677
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines [published correction appears in Hypertension. 2018 Jun;71(6):e140-e144]. Hypertension. 2018;71(6):e13-e115. doi:10.1161/HYP.0000000000000065
Age years
Gender
Race
Total Cholesterol mg/dL
HDL Cholesterol mg/dL
Systolic blood pressure mmHg
Treated for high blood pressure
Diabetes
Smoker